If left untreated, DVT can lead to complications such as pulmonary embolism, a potentially life-threatening condition. In this blog, we will delve into the causes, symptoms, risk factors, and treatment options for DVT, providing you with a comprehensive understanding of this condition.
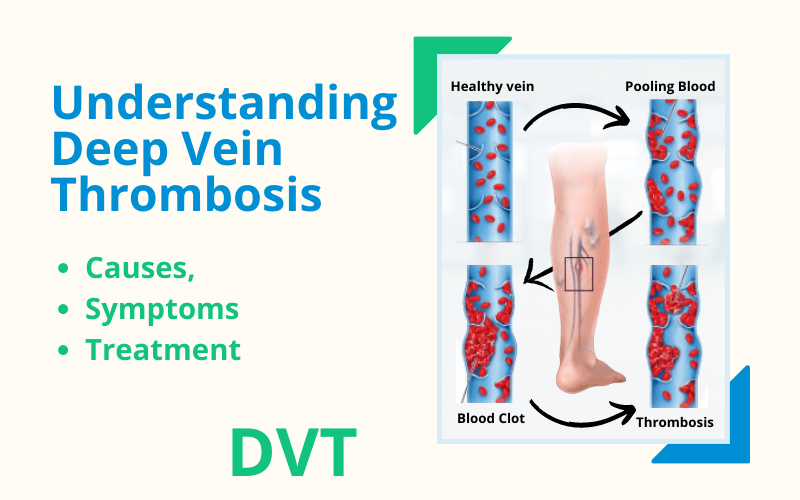
1. What is Deep Vein Thrombosis (DVT)?
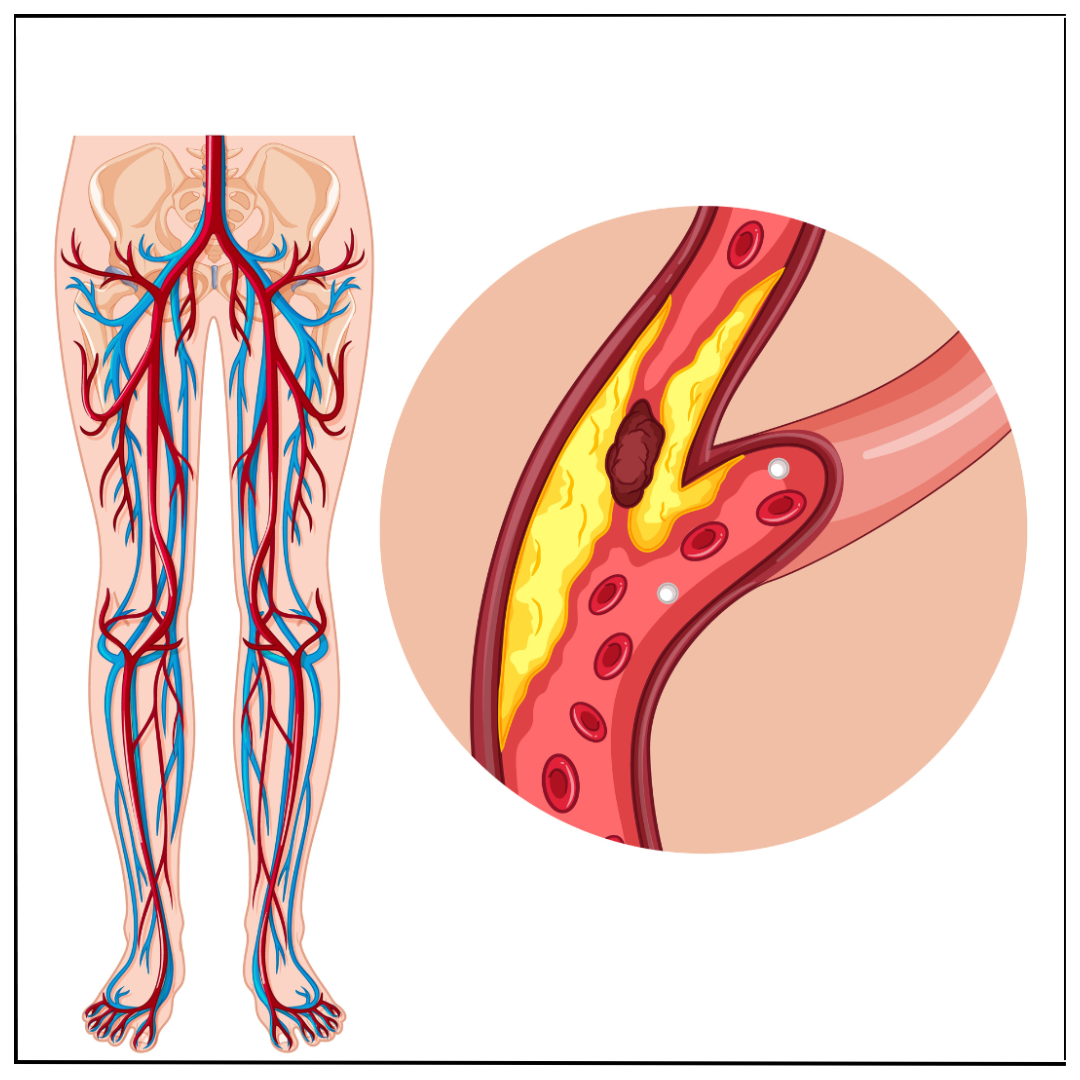
Deep Vein Thrombosis is the formation of a blood clot, or thrombus, in a deep vein, usually in the leg. It typically affects the large veins in the lower leg and thigh. The clot can partially or completely block blood flow, causing various symptoms and potential complications.
2. Causes and Risk Factors of DVT:
Several factors can contribute to the development of DVT. These include:
- Prolonged immobility: Sitting or lying down for long periods, such as during travel or hospitalization, can increase the risk of DVT.
- Surgery or trauma: Major surgery, especially involving the lower extremities, and trauma that damages blood vessels can trigger blood clot formation.
- Medical conditions: Certain medical conditions, such as cancer, heart failure, and inflammatory bowel disease, can increase the risk of DVT.
- Hormonal factors: Hormonal changes during pregnancy, use of oral contraceptives, or hormone replacement therapy can make individuals more susceptible to DVT.
- Genetics: Inherited blood-clotting disorders can predispose individuals to develop abnormal blood clots.
- Age and obesity: The risk of DVT tends to increase with age, and obesity can further elevate this risk.
3. Symptoms and Diagnosis of DVT:
Recognizing the symptoms of DVT is crucial for early diagnosis and treatment. Common symptoms include:
- Swelling in the affected leg, usually in the calf or thigh.
- Pain or tenderness, often described as a cramp or soreness.
- Warmth and redness over the affected area.
- Enlarged, visible veins.
- Some individuals may experience no symptoms, making it important to be aware of risk factors and seek medical attention if any concerns arise.
Diagnosing DVT typically involves a combination of the following:
- Medical history and physical examination: Your healthcare provider will assess your symptoms, medical history, and perform a physical examination to check for signs of DVT.
- Ultrasound imaging: This non-invasive test uses sound waves to visualize the veins and identify the presence of blood clots.
- D-dimer test: A blood test that measures the levels of a specific substance produced when a blood clot dissolves. Elevated levels can indicate the possibility of a clot.
4. Complications and Prevention of DVT:
If a DVT is left untreated, it can lead to complications, the most serious being a pulmonary embolism (PE). A PE occurs when a clot breaks free from the vein and travels to the lungs, blocking blood flow and potentially causing significant damage.
To reduce the risk of DVT, consider the following preventive measures:
- Maintain an active lifestyle: Regular exercise can improve blood circulation and reduce the risk of blood clots. Incorporate activities such as walking, swimming, or cycling into your routine.
- Move during prolonged periods of immobility: If you have to sit or stand for long periods, take breaks to stretch your legs and move around. Simple leg exercises, such as ankle flexion and extension, can help promote circulation.
- Stay hydrated : Proper hydration can help prevent blood from becoming too thick and reduce the risk of clot formation.
- Compression stockings: If you are at a high risk of DVT, your healthcare provider may recommend wearing compression stockings to improve blood flow in the legs.
- Medication and interventions: In some cases, individuals at high risk of DVT may be prescribed blood-thinning medications or undergo preventive procedures prior to surgeries or prolonged immobility.
5. Treatment Options for DVT:
The primary goals of DVT treatment are to prevent the clot from growing, reduce the risk of complications, and prevent future blood clots. Treatment options include:
- Anticoagulant medications: These medications, commonly known as blood thinners, help prevent the clot from getting larger and reduce the risk of new clots forming. They may be prescribed in the form of injections or oral tablets.
- Thrombolytic therapy: In certain cases of severe DVT, thrombolytic therapy may be used. It involves administering medications that can dissolve blood clots quickly. Options of thrombolytic therapy include pharmacomechanical thrombectomy using angiojet, thrombosuction using penumbra suction device, catheter directed thrombolysis and rarely systemic thrombolysis.
- Inferior vena cava (IVC) filters: In rare situations where anticoagulant therapy is not possible or effective, a small device called an IVC filter may be inserted into the inferior vena cava (the large vein that carries blood from the lower body to the heart). The filter helps prevent clots from reaching the lungs. After the work of IVC filter is done, it is recommended to remove it as soon as possible (usually within a month), or else the risk of compliucations increases and it becomes impossible to remove the filter.
- Compression therapy: Compression stockings or bandages can be used to improve blood flow and reduce swelling in the affected leg.
6. Long-term Management and Follow-up:
After the initial treatment of DVT, long-term management is crucial to prevent recurrence. This may involve the continued use of anticoagulant medications for a specified duration and implementing lifestyle modifications to address underlying risk factors. Regular follow-up appointments with your healthcare provider are essential to monitor your condition and adjust the treatment plan if necessary.
Conclusion:
Deep Vein Thrombosis is a potentially serious condition that requires prompt diagnosis and appropriate treatment. By understanding the causes, recognizing the symptoms, and adopting preventive measures, you can reduce the risk of DVT. If you suspect you may have DVT or have concerns about your vein health, consult with the nearest vascular surgeon for a comprehensive evaluation and personalized treatment plan.
Remember, this blog is intended for informational purposes only and should not replace professional medical advice.




 What You Need to Know.jpg)

.png)
