For patients with kidney failure, dialysis serves as a lifeline. Central to effective dialysis treatment is a well-functioning vascular access, a crucial step that often involves the creation of an arteriovenous fistula (AVF). This article aims to provide an in-depth understanding of what an arteriovenous fistula is, its benefits, and how to care for it.
What is an Arteriovenous Fistula (AVF)?
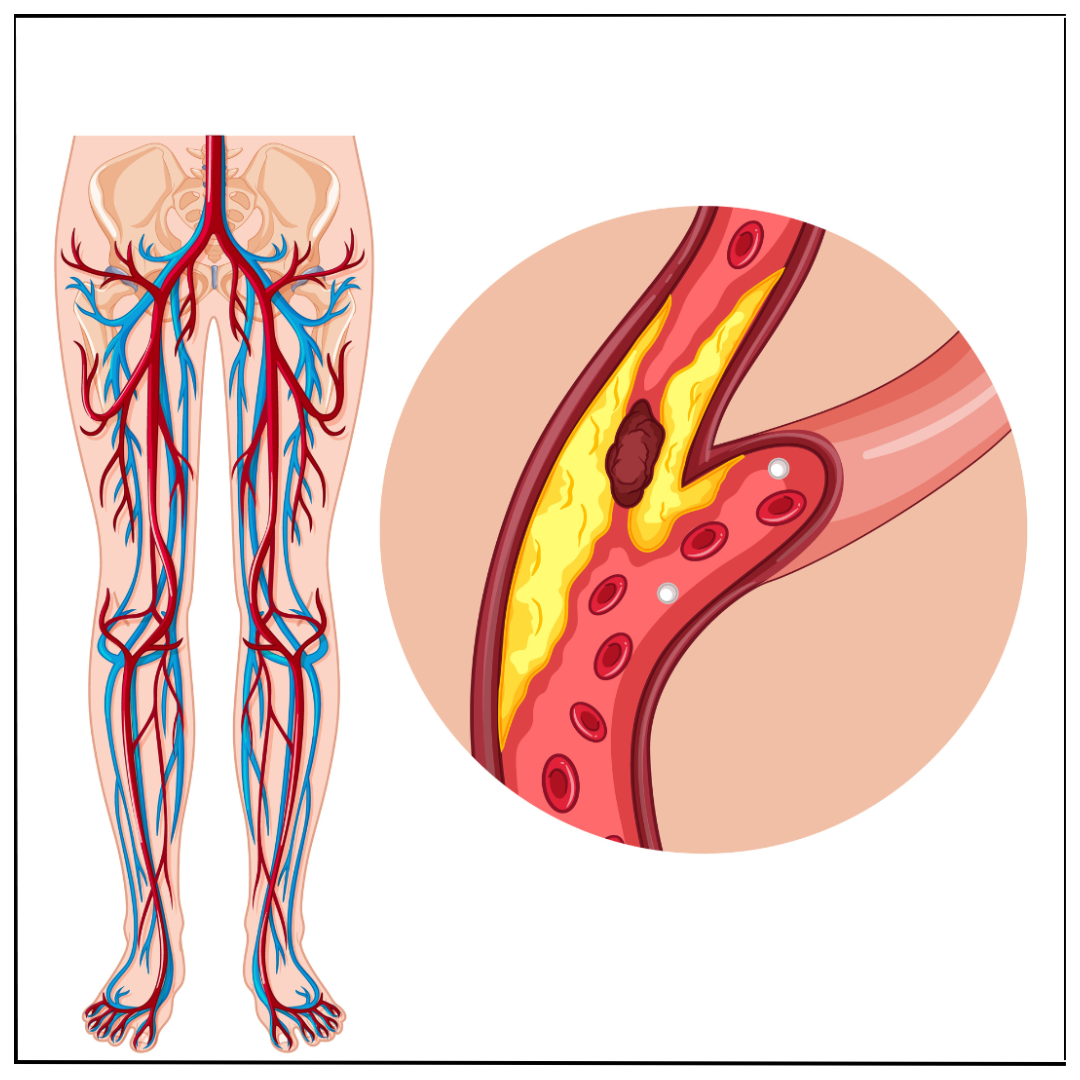
An arteriovenous fistula is a surgical connection made between an artery and a vein. This connection is typically created in the upper limb (forearm or arm) and allows for easy access to the bloodstream for dialysis. The increased blood flow resulting from the connection causes the vein to grow stronger and larger over time, making it suitable for repeated needle insertions required during hemodialysis sessions. The maturation process ensures the vein becomes robust enough to handle the high blood flow required for effective dialysis.
Why Is an Arteriovenous Fistula Recommended for Dialysis?
Arteriovenous fistulas are often considered the gold standard for vascular access in dialysis for several reasons:
- Durability: An arteriovenous fistula can last for many years if properly cared for, unlike other forms of access, such as catheters or grafts. This longevity reduces the need for repeated surgeries and interventions.
- Lower Risk of Infection: Because an arteriovenous fistula is created using the patient’s own blood vessels, the risk of infection is significantly reduced compared to synthetic options or catheters, which can serve as entry points for bacteria.
- Better Blood Flow: Arteriovenous fistulas provide optimal blood flow, ensuring effective and efficient removal of toxins and excess fluid during dialysis sessions. This enhanced efficiency can improve patient outcomes and overall health.
- Fewer Complications: Arteriovenous fistulas have a lower risk of clotting compared to synthetic grafts or catheters, making them a safer and more reliable choice.
Who Can Get an Arteriovenous Fistula?
Not all patients are candidates for an arteriovenous fistula. Your doctor will evaluate your:
- Blood Vessel Health: Healthy veins and arteries are necessary for a successful arteriovenous fistula. Ultrasound imaging is often used to assess the condition of your blood vessels before surgery.
- Age and Overall Health: Some patients may not be suitable for surgery due to underlying conditions such as severe cardiovascular disease or poor wound healing.
- Dialysis Timeline: An arteriovenous fistula needs time (4-8 weeks) to mature before it can be used, so it’s best suited for planned dialysis. If dialysis is urgently needed, a temporary catheter may be used initially.
The Procedure: What to Expect
Creating an arteriovenous fistula is a straightforward outpatient surgical procedure. Here is what typically happens:
- Pre-Surgical Assessment: The surgeon examines your arm using ultrasound to identify the best blood vessels for the fistula. Factors like vessel size, depth, and flow are taken into account.
- Surgery: Under local or regional anesthesia, the surgeon connects an artery and a vein. This connection allows arterial blood to flow directly into the vein, increasing its size and strength over time. The procedure usually lasts 1-2 hours.
- Recovery: You may experience mild discomfort or swelling, which subsides in a few days. Follow your doctor’s instructions for care and activity restrictions. Avoid strenuous activities or heavy lifting with the affected arm during the initial healing phase.
Caring for Your Arteriovenous Fistula
Proper care is essential to ensure the longevity and functionality of your arteriovenous fistula. Follow these tips:
Daily Monitoring
- Check for the Thrill: Gently place your fingers over the fistula to feel a vibration (known as a “thrill”). This indicates proper blood flow through the arteriovenous fistula. If the thrill feels weaker than usual or is absent, contact your vascular surgeon immediately.
- Inspect for Changes: Look for redness, swelling, or pain, which could signal infection or blockage. Early detection of complications can prevent more serious issues.
Hygiene
- Keep It Clean: Wash the area daily with soap and water to minimize the risk of infection. Ensure the skin around the arteriovenous fistula remains dry and clean.
- Avoid Infections: Do not scratch or puncture the skin around the arteriovenous fistula. Inform your healthcare team if you notice any signs of infection, such as warmth, redness, or pus.
Avoid Pressure
- No Tight Clothing: Avoid wearing tight sleeves or jewelry on the arm with the arteriovenous fistula. Constrictive items can impair blood flow and damage the fistula.
- No Heavy Lifting: Prevent strain on the arm to reduce the risk of damage. If you need to lift objects, use the unaffected arm. However, small weights up to 2-3 kgs is fine.
Regular Follow-Up
Routine check-ups with your vascular surgeon are crucial to monitor the health of your arteriovenous fistula. Your medical team may perform tests, such as ultrasound or physical exams, to ensure the fistula remains functional.
Common Complications and How to Address Them
While arteriovenous fistulas are generally safe and reliable, complications can occasionally occur. Be aware of these common issues:
- Infection: Symptoms include redness, warmth, or discharge. Seek medical attention immediately if you notice these signs, as untreated infections can spread and become severe.
- Clotting: A sudden loss of the thrill or bruit (sound heard with a stethoscope) could indicate a blood clot. Immediate intervention is required to restore blood flow.
- Steal Syndrome: This rare complication occurs when too much blood is diverted from the hand, causing pain, coldness, or numbness. Treatment may involve surgical correction to restore balance.
- Aneurysm Formation: Over time, the vein at the fistula site can become enlarged or bulge. Regular monitoring can help detect this issue early, and surgical repair may be necessary.
Conclusion
An arteriovenous fistula is a vital step in ensuring effective and reliable dialysis treatment. By understanding its importance, the procedure involved, and the necessary aftercare, patients can take proactive steps toward better health outcomes. The durability, low risk of infection, and superior blood flow make an arteriovenous fistula the preferred choice for vascular access in dialysis patients.
If you or a loved one is considering dialysis, consult with a qualified nephrologist and vascular surgeon to determine the best vascular access option for your needs. Your healthcare team will guide you through the process to ensure the best possible care and outcomes.
For booking an appointment or to learn more, contact Dr. Rahul Agarwal today!





 What You Need to Know.jpg)

.png)
