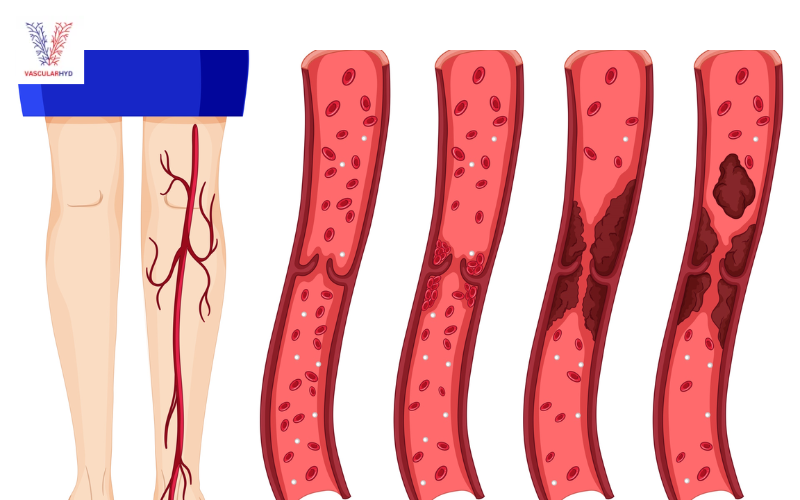
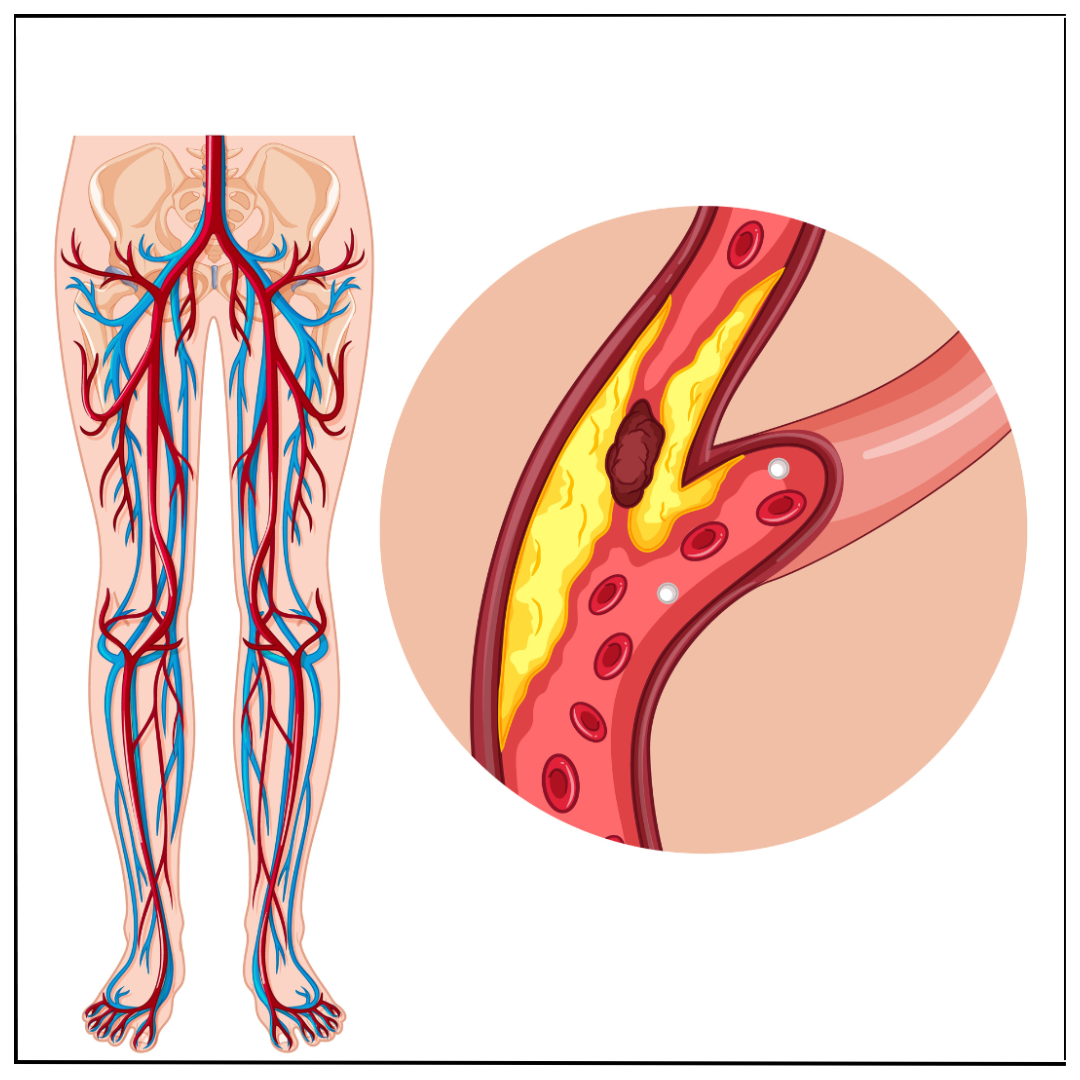
Why Managing PAD Naturally Is Important
PAD is not only a leg problem—it’s a warning sign of more widespread arterial disease, which increases the risk of heart attack and stroke. Adopting healthy habits can:
- Improve blood flow to your legs
- Reduce the need for surgery
- Enhance walking ability and stamina
- Lower your cardiovascular risk
- Support long-term wellness
Natural management is especially effective when combined with the guidance of a vascular surgeon.
1. Quit Smoking Immediately
Smoking is one of the most significant risk factors for PAD. It damages blood vessels, promotes plaque buildup, and accelerates arterial narrowing.
Quitting smoking can:
- Improve circulation
- Slow disease progression
- Enhance the effectiveness of treatments
- Lower the risk of heart disease and stroke
If you need help, I can recommend smoking cessation programs and support resources as part of your PAD care plan.
2. Get Moving: Structured Exercise Program
Exercise is one of the most effective natural treatments for PAD. Even if walking is painful, supervised walking therapy improves circulation and trains muscles to use oxygen more efficiently.
Tips for getting started:
- Begin with short walks (5–10 minutes) and gradually increase
- Stop when pain starts, rest, then continue
- Aim for 30–45 minutes of walking, at least 3–5 times a week
- Avoid high-impact activities; low-impact exercises like cycling or swimming are great alternatives
I often recommends customized exercise therapy that fits your fitness level and health status.
3. Eat a Heart-Healthy, Anti-Inflammatory Diet
Nutrition plays a powerful role in managing PAD and cardiovascular disease. A Mediterranean-style diet rich in whole foods helps reduce inflammation, cholesterol, and blood pressure.
Recommended Foods:
- Leafy greens (spinach, kale)
- Whole grains (brown rice, oats)
- Fatty fish (salmon, mackerel)
- Olive oil, nuts, and seeds
- Berries and other colorful fruits
- Low-fat dairy and lean proteins
Avoid:
- Processed foods
- Sugary drinks
- Saturated and trans fats
- Excess sodium
I work with a dietitian to design a meal plan that supports your vascular health goals.
4. Manage Blood Sugar, Blood Pressure, and Cholesterol
PAD often coexists with diabetes, hypertension, and high cholesterol—conditions that worsen arterial damage. Natural management strategies include:
- Limiting sugar and refined carbs
- Reducing salt intake
- Increasing fiber and plant-based foods
- Managing stress with yoga, meditation, or deep breathing
In some cases, medication may be needed to keep these levels in check. I carefully monitors these metrics to reduce the risk of complications.
5. Maintain a Healthy Weight
Obesity contributes to inflammation, high cholesterol, and elevated blood pressure—all of which aggravate PAD. Even modest weight loss can improve symptoms and reduce strain on the circulatory system.
Try to:
- Set realistic weight-loss goals (5–10% of body weight)
- Track your food intake
- Stay physically active
- Get adequate sleep (7–8 hours/night)
I emphasize a holistic approach that supports lasting lifestyle changes rather than quick fixes.
6. Foot and Leg Care Matters
PAD can reduce blood supply to your feet, increasing the risk of sores, infections, or ulcers that heal poorly.
Daily Foot Care Tips:
- Inspect your feet for blisters, cuts, or color changes
- Keep feet clean and moisturized
- Avoid walking barefoot
- Wear properly fitting shoes
- Trim toenails carefully to avoid injury
I provide wound care services and vascular access solutions at VascularHyd for PAD patients at risk of foot complications.
7. Natural Supplements (Only Under Medical Guidance)
Some supplements may support blood flow and reduce inflammation, such as:
- Omega-3 fatty acids
- Vitamin D
- Coenzyme Q10
- L-arginine
However, not all supplements are safe or effective. Always consult your vascular specialist before starting any new supplement—especially if you're taking blood thinners or managing chronic conditions.
When Lifestyle Changes Aren’t Enough
While lifestyle changes are foundational, some patients require advanced treatment to manage symptoms and prevent complications. I offer:
- Doppler ultrasound diagnostics
- Angiography and angioplasty
- Endovascular interventions
- Stent placement
- Bypass procedures (if necessary)
With early detection and timely care, many PAD patients can avoid surgery and live full, active lives.
Take the First Step Toward Better Vascular Health
Peripheral Arterial Disease doesn't have to limit your life. With natural lifestyle changes and expert medical care you can take control of your symptoms and protect your long-term health.
- Read more in our other blogs about peripheral artery disease and varicose veins.




.png)

 (1).png)