Most people experience leg pain at some point in their lives. Whether from exercise injury or fatigue, leg discomfort is common — and often harmless. But what if that pain is trying to tell you something more serious? If you frequently experience cramping numbness or aching in your legs while walking or at rest it may not just be soreness. It could be a warning sign of Peripheral Artery Disease (PAD).
In this blog we’ll explain what PAD is, how to recognize the difference between regular leg pain and vascular related discomfort and why early diagnosis is crucial to preventing serious health complications.
What is Peripheral Artery Disease (PAD)?
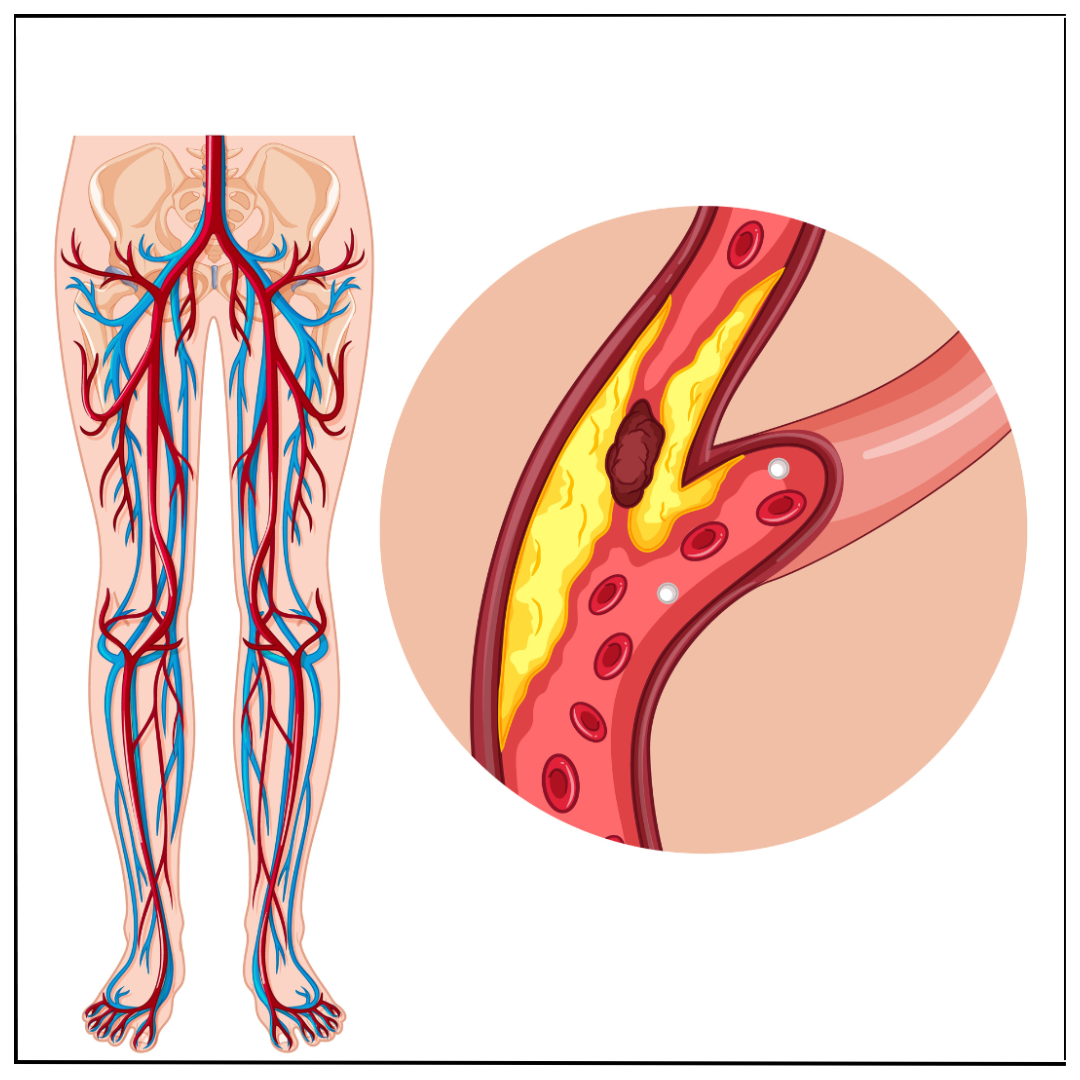
Peripheral Artery Disease (PAD) is a common circulatory condition where narrowed arteries reduce blood flow to the limbs, usually the legs PAD is primarily caused by atherosclerosis — the buildup of fatty deposits (plaque) in the artery walls — which restricts blood circulation.
When your leg muscles don’t receive enough oxygen rich blood especially during physical activity it leads to pain, cramping or fatigue most often in the calves, thighs or hips.
PAD is not just about leg pain — it's a systemic vascular disease that increases your risk of heart attack stroke and limb amputation if left untreated.
Is It Just Leg Pain or PAD? Know the Difference
Many people dismiss leg discomfort as a part of aging dehydration or simple overuse. But PAD related leg pain also known as claudication has some distinct characteristics :-
1 Pain While Walking (Intermittent Claudication)
- Leg pain that starts when you walk or climb stairs but stops with rest is a hallmark symptom of PAD
- It often occurs in the calves but may also affect the hips, buttocks or thighs
2 Rest Pain in Severe PAD
- As PAD worsens you may feel pain in your legs or feet even at rest especially at night
- Hanging your legs over the side of the bed may relieve the discomfort
3 Coldness or Numbness in the Legs or Feet
- If one leg feels significantly colder or numb compared to the other, reduced blood flow could be the cause
4 Slow Healing Wounds on Feet or Toes
- Ulcers or sores that don't heal properly can indicate critical limb ischemia — a severe form of PAD
5 Shiny Skin Hair Loss or Weak Pulse in the Legs
- These subtle skin and vascular changes often accompany decreased circulation in the legs
Risk Factors for PAD
Understanding your risk profile can help you take action early. You are at a higher risk of developing PAD if you have :-
- Diabetes
- High blood pressure
- High cholesterol
- Smoking
- Obesity or sedentary lifestyle
- Family history of cardiovascular disease
- Age above 50 especially with other risk factors
PAD is more than just a leg condition — it reflects widespread vascular disease and must be addressed holistically.
Why Early Detection of PAD Matters
Many people live with PAD for years without realizing it. Unfortunately when symptoms are ignored the disease progresses silently.
Complications of untreated PAD include :-
- Increased risk of heart attacks and strokes
- Gangrene or tissue death in the legs
- Limb amputation
- Reduced mobility and quality of life
The good news is that PAD can be effectively managed — especially when caught early.
How PAD is Diagnosed
If you're experiencing unexplained leg pain or suspect PAD consulting a vascular specialist is crucial Diagnosis often includes :-
1 Ankle Brachial Index (ABI)
- A non-invasive test comparing blood pressure in your ankle and arm
- An abnormal result suggests reduced blood flow to your legs
2 Doppler Ultrasound
- Uses sound waves to assess blood flow in leg arteries
3 CT Angiography or MR Angiography
- Provides detailed images of arteries to locate blockages or narrowing
These tests are painless and offer valuable insight into your vascular health.
Treatment Options for PAD
Treating PAD depends on its severity but the goals remain the same : improve blood flow, reduce symptoms and prevent progression.
Lifestyle Changes
- Quit smoking — the #1 preventable risk factor for PAD
- Exercise regularly especially walking programs to improve circulation
- Adopt a heart healthy diet low in saturated fats and cholesterol
- Control diabetes and blood pressure
Medications
- Blood thinners to reduce clotting risk like ecosprin and clopidogrel
- Cholesterol lowering drugs like statins
- Medications to improve walking distance and relieve symptoms like cilostazol
Minimally Invasive Procedures
Our vascular specialists use advanced endovascular techniques to restore blood flow with minimal discomfort and faster recovery times. These procedures are typically performed through small incisions, avoiding the need for open surgery.
-
Angioplasty
A small balloon-tipped catheter is guided into the narrowed or blocked artery. Once in place, the balloon is gently inflated to widen the artery and improve blood flow. After dilation, the balloon is deflated and removed.
-
Stent Placement
Often combined with angioplasty, a stent—a small mesh tube—is placed inside the artery to keep it open. This helps prevent the artery from narrowing again, ensuring long-term vessel patency.
- Atherectomy
In this procedure, plaque buildup is physically removed from the artery walls using a specialized device. Atherectomy may be recommended for hard or calcified blockages that are difficult to treat with angioplasty alone.
Open Surgical Procedures
For complex or advanced vascular conditions, open surgery remains the gold standard. These procedures involve direct access to the blood vessels and are often chosen when minimally invasive options are not suitable.
-
Bypass Surgery
A new pathway is created for blood to flow around a blocked artery. This is done using either a vein from the patient's own body or a synthetic graft. Commonly performed for leg arteries (femoral-popliteal bypass) or in major vessels like the aorta.
-
Endarterectomy
Plaque buildup is surgically removed from the inner lining of an artery. The most common form is carotid endarterectomy, used to prevent stroke in patients with significant narrowing of the carotid arteries.
-
Aneurysm Repair
A weakened or bulging section of an artery (aneurysm) is replaced or reinforced. In open repair, the surgeon accesses the artery directly and replaces the aneurysmal segment with a synthetic graft. Often used in abdominal or thoracic aortic aneurysms.
Don’t Ignore Leg Pain — Get a Vascular Assessment Today
Leg pain may seem minor but when caused by Peripheral Artery Disease it’s a serious health warning. The earlier you detect and treat PAD the better your chances of preventing disability or life threatening complications.
Meet Dr Rahul Agarwal : Your Trusted Vascular & Endovascular Specialist in Hyderabad
If you suspect your leg pain may be more than just fatigue it's time to consult an expert Dr Rahul Agarwal a leading Vascular and Endovascular Specialist in Hyderabad offers comprehensive care for PAD and other vascular conditions.
With years of experience and expertise in diagnosing and treating vascular diseases using advanced minimally invasive techniques Dr Agarwal has helped countless patients regain their mobility, avoid complications and live healthier lives.
At vascularHYD you receive :-
- Expert evaluation and diagnosis
- Personalized treatment plans
- Access to advanced endovascular procedures
- Compassionate and results driven care
Book Your Consultation Today
Don’t ignore the warning signs. If you’re experiencing persistent or unusual leg pain, schedule a consultation with Dr Rahul Agarwal and take the first step toward better vascular health.
 (1).png)




 What You Need to Know.jpg)

.png)
